The massive, irreparable tearIf you have had shoulder problems for a long-time but managed the symptoms, you may have been harbouring a large tear in the tendon (cuff) in the shoulder. Some people can compensate very well which means they use other muscles which are working satisfactorily, to overcome the deficiencies in others. There may be a new, relatively moderate, injury which leads to a rapid decline in shoulder function and prompt a referral to see a surgeon. It may then be discovered that actually you have a chronic tear which has become so large and retracted that it is not repairable. The massive, irreparable tear continues to be a huge challenge for shoulder surgeons. The options are outlined below. Of course, not all options are always appropriate for all patients.
Non operative treatmentYou don’t necessarily need to have anything surgically done. If you can tolerate the symptoms then many patients go on for years without deteriorating. Some may improve marginally over a period of time. A good place to start would be some physiotherapy. There is a special physio regime called ‘anterior deltoid retraining’ which specifically strengthens the front of the deltoid muscle and aims to take-over the role of the superior cuff muscle which has been lost. It can work well but perseverance is definitely required. It may take 6 months before any improvement is noted so one needs to be determined and persistent at the daily exercises. One can consider steroid injections to help with pain but I would only recommend a few injections and then really they tend become less effective each time anyway. I would recommend injection therapy only in conjunction with a guided physiotherapy programme.
Operative treatmentPartial repairIt may be possible to repair part of the cuff. Many studies in the literature have shown that partial repair can lead to some improvement, especially of subscapularis (the tendon at the front), thought to be the most important of the cuff tendons. Also, if some of the posterior cuff can be brought up on to the top of the shoulder then this alone could be enough to improve symptoms. Again, physio plays a huge role is rehabilitation and outcome.
DebridementIf it isn’t possible to repair any of the cuff then just a general tidy-up in joint may help. It is often called a debridement which means ‘to clean’. This is done arthroscopically and is done under general anaesthetic. From personal experience this leads to improvement in about 50% of cases. The other 50% fail to gain much, if any, improvement from the procedure. The good news is, patients aren’t usually worse and you haven’t ‘burnt any bridges’ in terms of future treatment if it doesn’t work.
Subacromial BalloonThe subacromial balloon spacer (InSpace balloon) is an interesting concept where a small polyethylene balloon is inserted between the humeral head and the acromion (the roof of the shoulder). It is inserted under general anaesthetic and inflated with saline (water) inside the body. The aim is to act as a spacer to re-centre the head on the socket. Physiotherapy should take place soon after insertion to exercise deltoid. The balloon gets absorbed by the body at about 3 months after insertion so there isn’t long to get that physio to work. Again, the results are mixed. It may work well to reduce pain but it doesn’t tend to make a difference to range of movement. Of course, it may have no effect at all. I think the technique is best described as 'experimental'. It isn't harmful, but the results are mixed. You can watch a video about it here https://www.youtube.com/watch?v=GDYKUBBZ2Ks
PatchesThere are various types of patches available on the surgical market. They can be synthetic, from pig skin or donated human skin. This concept can be split into two main applications. It can be used to reinforce a repaired cuff, so called augmentation, or to literally patch a hole (called interposition) where it acts as a bridge. My preference for patch use would tend to be only for augmentation when the repair is possible but the tendon is a little thin and fragile. I think it is a lot to expect of a patch to bridge across a defect in the cuff. I use the LeedsKuff patch, see image to the right (https://www.neoligaments.com/product/leeds-kuff-patch/) which is manufactured in Leeds and I sew it into the tendon in an open approach (not key-hole) to the shoulder. The cut is about 6 cm long and is on the side of the shoulder and goes through the deltoid muscle. My results are generally good. It certainly won’t return you to normal shoulder function but it may give reduced pain levels and some modest improvement in function (movement). I would call this a salvage operation, which means I’m trying to buy you a few years before anything more radical, like a shoulder replacement, may be necessary. 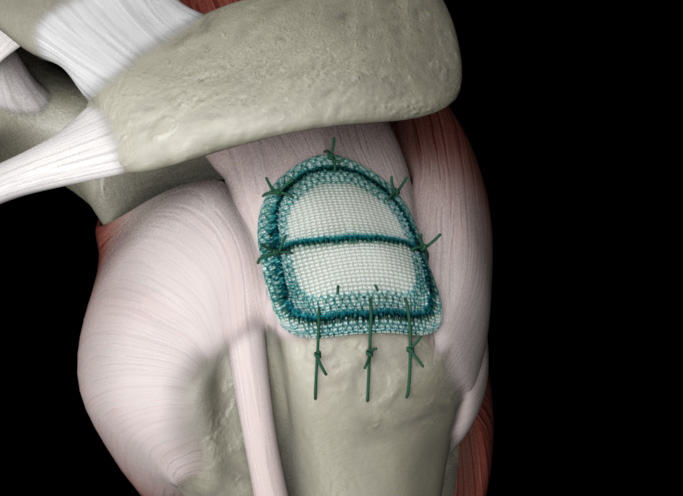
Muscle transferThis is not something that I offer but it is feasible in very definable circumstances. In the broadest terms, a muscle that is functioning well around your shoulder (the latissimus dorsi) is detached from its natural position and transferred onto the head of the humerus. The intention is that it functions in a similar fashion to the muscle that it is replacing. Generally you will not suffer much loss from having the muscle moved. The problem is that the new muscle won’t function in exactly the same way as the muscle it replaces. There will always be a deficiency. Rehabilitation with physio is critical and probably the key to success. It is complex surgery and is only offered in a few centres in the UK. One of the biggest factors is that the shoulder must have no (or almost no) degenerative change (arthritis) and by the time the cuff has torn this much that a muscle transfer might be required, usually there is some arthritis.
SCRSuperior capsule reconstruction (SCR) is a novel treatment option for massive, irreparable rotator cuff tears. Treatment goals of are to reduce pain, restore shoulder function and delay the development of advanced cuff tear arthropathy. SCR is a promising alternative treatment using a bridging graft from the superior glenoid (socket) to the greater tuberosity (top of the humeral head) to stabilise the humeral head. In the image on the right, the graft is the cream-coloured section stitched into the red muscle. It is not dynamic; it doesn’t contract. It is purely a taught band which aims to stop the humeral head rising up when deltoid contracts. It has been described as a reverse-trampoline. It was introduced to the west by Dr Mihata from Japan who, in the early 2000’s was using it to treat cuff deficiencies as the reverse arthroplasty wasn’t easily available. He used fascia lata (a tendon found in the thigh) and transferred it into the shoulder. In Europe it is more common to use human donor skin (graft). The skin is fully cleaned, sterilised and free from disease. The piece we start with is about 10 x 5 cm and is cut down to suit the patient. It is about 4mm thick and can be introduced into the shoulder and stitched in place via key-hole surgery. NICE guidelines state that it is experimental and should only be undertaken as part of research. If you undergo this procedure under my care, I will be asking you to complete some questionnaires to assist surgeons learn more about this technique and its outcomes. Early outcomes in our series have been promising and we now have cases greater than 18 months from surgery with continued excellent clinical and structural results. Pain relief is typically marked and occurs surprisingly early. Functional improvement can take a while. I would say it takes a year before a true outcome can be measured. 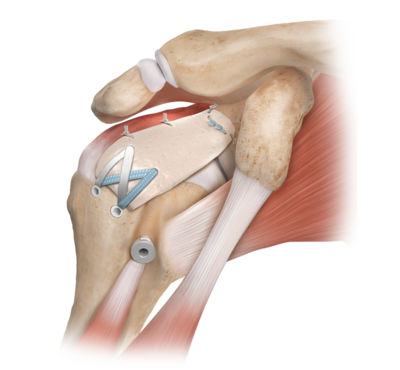
This video shows a patient of mine on whom I have performed a RIGHT shoulder superior capsular reconstruction. Asyou can see he has excellent shoulder movement and it almost matches the normal LEFT shoulder.
Suprascapular nerve blocks / ablationThe suprascapular nerve carries pain messages from the shoulder to the spinal cord. It is also responsible for motor function of part of the rotator cuff (supraspinatus and infraspinatus). Once the supraspinatus and infraspinatus are completely torn, they are not functioning anyway. Once it is established that they will never be repaired, one can consider ablating (destroying) the nerve as its only remaining function is transmission of pain. The nerve in the image is the yellow cord and you can see that it travels under a ligament (white/grey strand) and then gives motor supply to the muscle (red). Usual practice would involve trialling an injection of steroid around the nerve first. If this gave good relief of pain then an ablation could be considered with the expectation that the same result as the injection would be achieved. The nerve can be ablated either via arthroscopic surgery or by radio-frequency (ultra-sound) and the method in each patient would need to be individualised. It is ablated at the point it travels under the ligament. 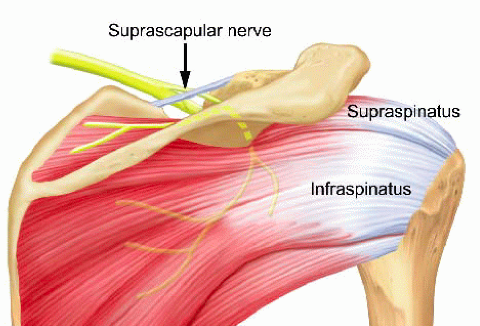
|