INSTABILITY
WHAT IS A SHOULDER DISLOCATION?
The shoulder joint is made up of the humeral head (the ball) and the glenoid (the socket). Unlike the hip joint, which is a round ball in a round socket, the shoulder is a round ball on a small, flat plate. It has been likened to a golf ball on a tee. This allows the huge range of movement that we benefit from in the joint but means it is susceptible to dislocation (coming out of joint) and subluxation (nearly coming out of joint).
There are several mechanisms which help keep the shoulder in joint. There is the glenoid labrum which is a thick rim of cartilage which runs around the rim of the glenoid and aims to deepen the plate to make it more cupped. There are ligaments which are like reins and become tight in certain positions of shoulder movement. Also, the rotator cuff muscles act as strong stabilisers pulling the head towards the socket.
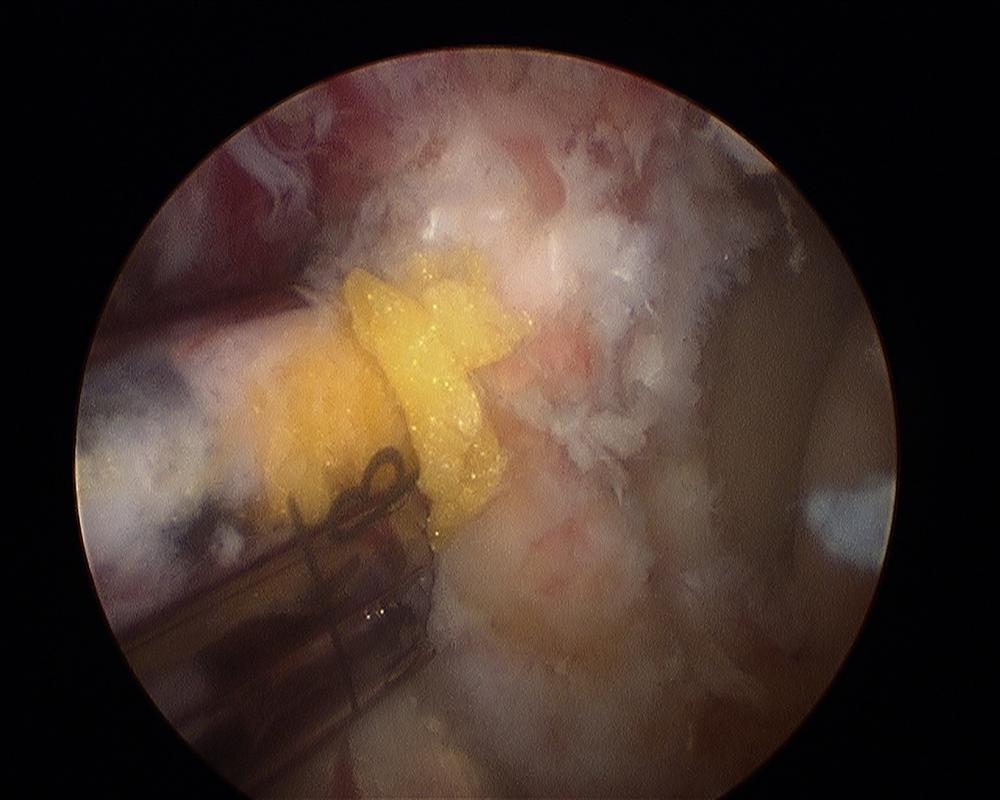
Arthroscopic Latarjet procedure. On the left is the cannula which allows the screws and screwdriver to be inserted safely down to the bone. On the right is the bone block against the anterior glenoid. On the far left is the glenoid articular cartilage. (courtesy of Dr L Lafosse, Annecy, France)
Arthroscopic Latarjet procedure. Bone block on anterior glenoid. On the left is the glenoid cartilage. In the centre is the bone block from the coracoid process and on the right is the screwdriver tightening the screws. (courtesy of Dr L Lafosse, Annecy, France)
If any of the mechanisms that usually keep the shoulder in check, stop functioning correctly, the shoulder can come away from the socket and come to lie either in front of the glenoid (anterior dislocation) or behind the glenoid (posterior dislocation). Rarely, the head can go under the glenoid (inferior dislocation). If the head moves out of its normal position but doesn’t quite part company from the glenoid, it is called a subluxation (a partial dislocation). The head returns to the normal position of its own accord but this can be painful.
The commonest position of dislocation is anterior. Posterior dislocations account for just 3% of dislocations and are more common in epileptics.
WHY DOES DISLOCATION OCCUR?Dislocation can be either traumatic (due to an injury) or atraumatic (no injury). If someone dislocates their shoulder due to a fall or accident, the structures that normally act to hold the head of the humerus on the socket get torn or fracture and are unlikely to recover normal function again. If a young (<30 years) person dislocates their shoulder during an injury, they have a very high chance of having future dislocations and the trauma required to dislocate the joint will be less each time.
Atraumatic dislocations occur due to a number of factors including joint laxity (stretchiness or being double-jointed) and loss of the normal synchronised pattern of movement of the muscles around the shoulder joint. People that have 'lax' joints, can often hyper-extend their knees and elbows and can get the palms of both hands onto the floor with their legs straight with ease. Whilst this joint laxity is normal for these people and something they have always had, the instability often arises when there is a change in how the muscles around the shoulder are interacting with each other or a change in posture/ position of the arm. The main treatment for this is physiotherapy although the physiotherapist will need to be specialists in treating patients with this condition. The physiotherapist will look at the way in which the muscles and shoulder joint are moving as well as the patient’s posture. The physiotherapist will aim to train the patient to re-sequence the muscles in order to prevent further dislocations. The patient has to be highly motivated and willing to undergo this treatment which takes many, many months of perseverance. The treatment can be very frustrating in the early stages as it takes lots of patience and application to reactivate these muscles which may have been ‘dormant’ for many months or even years.
WHAT CAUSES SHOULDER INSTABILITY?Shoulder instability often follows an initial injury that caused the shoulder to dislocate. This initial injury is usually fairly significant and the shoulder must be reduced (put back into place). To reduce a shoulder means it must be manually put back into the socket. The shoulder may seem to return to normal, but the joint often remains prone to further episodes of dislocation. The ligaments that hold the shoulder in the socket, along with the labrum (the cartilage rim around the glenoid), may have become stretched or torn.
This makes them too loose to keep the shoulder in the socket when it moves in certain positions. An unstable shoulder can result in repeated episodes of dislocation, even during normal activities. Instability can also follow less severe shoulder injuries.
In some cases, shoulder instability can happen without a previous dislocation. People who do repeated shoulder motions may gradually stretch out the joint capsule. This is especially common in athletes such as volleyball players and swimmers. If the joint capsule gets stretched out and the shoulder muscles become weak, the ball of the humerus begins to slip around too much within the shoulder.
Eventually this can cause irritation and pain in the shoulder. A genetic problem with the connective tissues (eg Ehlers Danlos) of the body can also lead to ligaments that are too elastic. When ligaments stretch too easily, they may not be able to hold the joints in place. All the joints of the body may be too loose. People with this condition are sometimes referred to as hyper-lax or ‘double-jointed’. Some people can even dislocate, and then relocate, their shoulder on demand as a 'party-trick'. This makes the problem worse and is strongly discouraged by specialists.
LaxityLaxity is the excessive 'looseness' of a joint. Many people will have known this as being 'double-jointed'. In itself, it is often not a problem (in fact, it is really a variant of normal) but it can predispose to instability (abnormal movement of a joint). It can be measured using the Beighton's score. A positive 'sulcus sign' as shown in the video is generally accepted as a sign of Multi-directional Instability (MDI). It is a sign of laxity around the shoulder. In the video I am dislacing the humeral head inferiorly on the glenoid (socket) and the vacuum draws in the skin, causing the 'sulcus'.
WHAT ARE THE SYMPTOMS?An acute shoulder dislocation due to an injury is very painful. The shoulder will look abnormal. The patient may also experience abnormal sensations in the hand which is due to pressure on the nerves in the area. Sometimes the shoulder will go back into the socket of its own accord but more commonly the patient would come to hospital to have medical assistance in reducing the shoulder back into position. Usually when the shoulder is back in position, the pain is much improved. Usually a sling is provided by the hospital for comfort but should only be worn for as long as the shoulder is painful and then dicarded, usually about a week. If the shoulder continues to come out of joint the patient will sense that their shoulder feels ‘loose’ and they are nervous about their shoulder being in certain positions (called apprehension).
HOW IS SHOULDER INSTABILITY DIAGNOSED?In the urgent situation of a shoulder dislocation the doctor will take a history, perform and examination of your shoulder and get an x-ray. Usually the x-ray shows the shoulder is out the socket and whether the ball has come to lie at the front or behind the socket. If your shoulder continues to come out of joint you may consult a shoulder surgeon. They will ask specific questions about when the shoulder first came out of joint and any episodes since. It is also important what sort of sports you like to get involved in and what job you do. Normally an x-ray will be requested on your shoulder. This will only show if there are problems with the bone and frequently the problem lies in the ligaments and other soft tissues surrounding the joint. To assess the soft tissues around the joint your surgeon may ask for you to have a CT or an MRI scan (commonly an arthrogram which involves an injection of a dye).
WHAT IS THE TREATMENT?
Nonsurgical Treatment:After an acute dislocation or episode the important thing is to control your pain and rest the joint. In the chronic situation, physiotherapy can help to strengthen the muscles which help to keep the joint in a normal position. If you are not involved in manual work, particularly over-head height and not involved in collision sports, you may only need physiotherapy to avoid further problems.
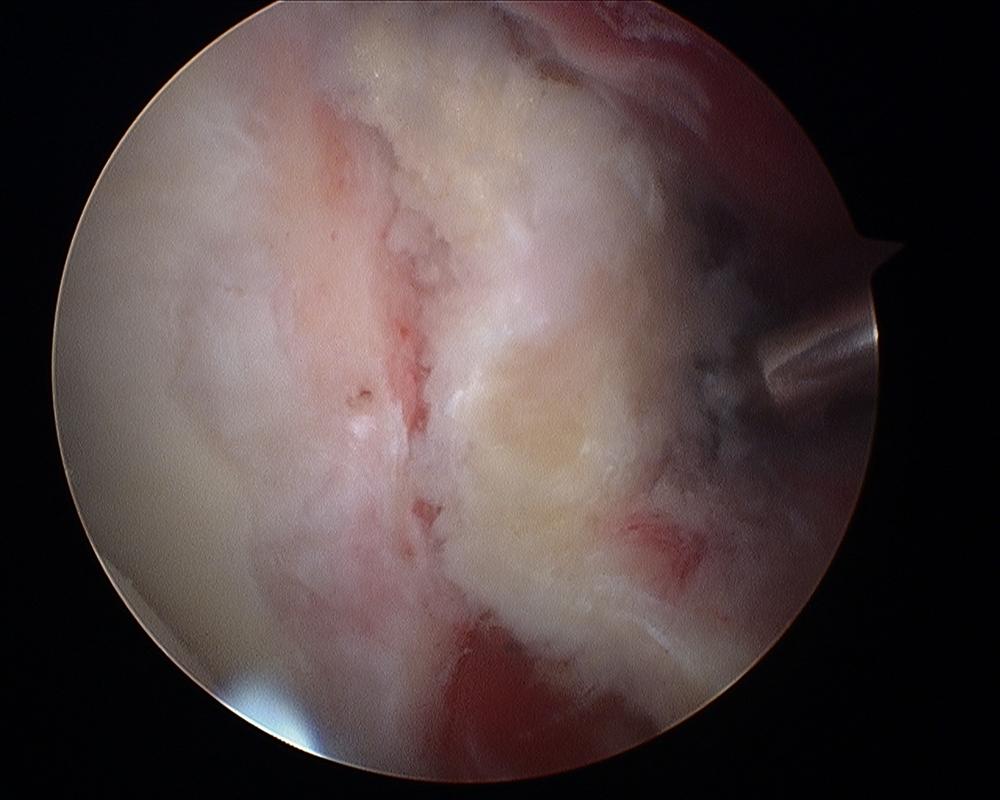
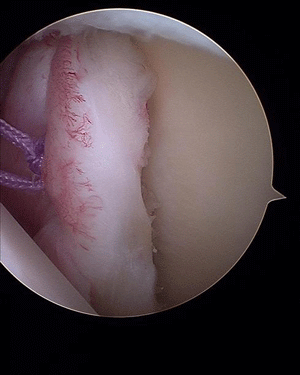
Bankart (anterior labral repair). The figure shows the repaired labrum with the suture knot behind, away from the joint articulation.
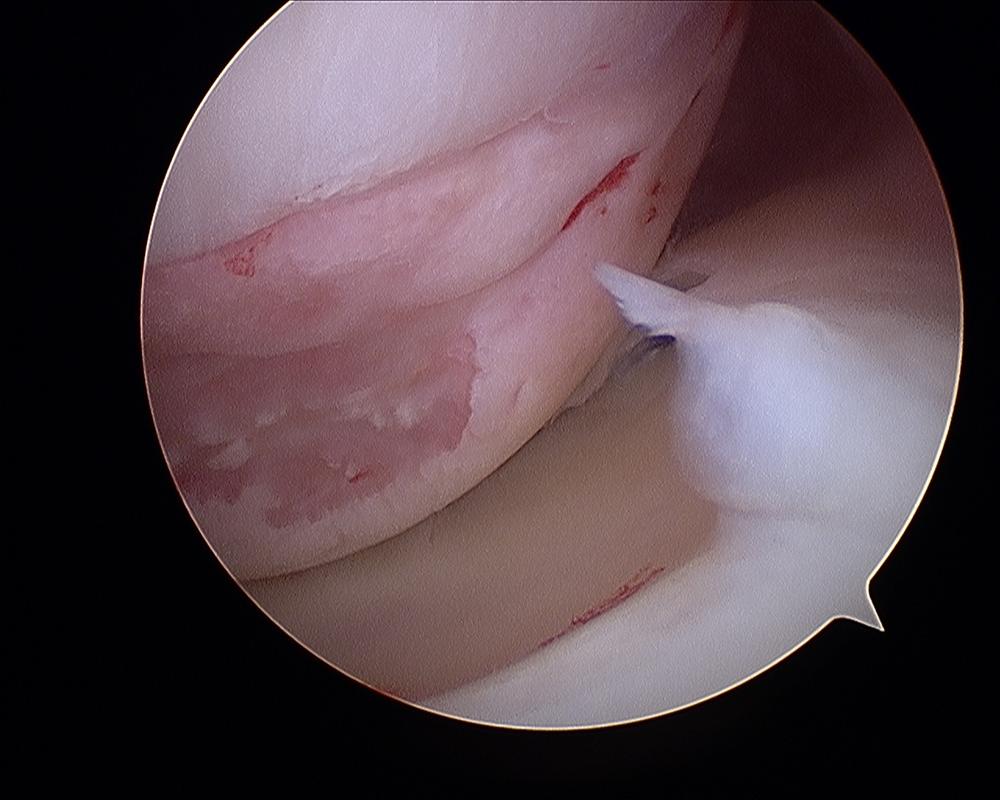
Hill-Sachs lesion (impaction fracture on posterior aspect of humeral head as a result of anterior dislocation)
Surgical treatment: If you have physiotherapy or your activity means that future dislocation is likely, you may be offered surgery. The type of operation depends on which direction (out the front or out the back), and the reason why your shoulder is dislocating. If the primary cause is damage to the ligaments and labrum (cartilage) at the front of the joint, the commonest operation is called a Bankart repair, which aims to reattach these structures back onto the bone. Traditionally this operation was done through an incision (a cut) on the front of the shoulder and required alot of normal tissue to be dissected (disturbed) in order for the damaged tissue to be repaired. Nowadays it is more common for the operation to be performed arthroscopically (via key-hole surgery). It is often a day-case operation, not even requiring a nights stay in hospital. The camera (about the size of a thin pen) is inserted into the back of the shoulder and instruments are passed into the front of the shoulder. Small anchors (screws with stitches on the end) are placed on the front of the joint and the soft tissue is stitched down to hold it in place whilst it heals. You will need sling for approximately 4 weeks after the surgery in order to rest the shoulder and allow the healing to start. This may well be sufficient to keep your shoulder stable.
Sometimes not only is the tissue on the front of the joint damaged but there is also some damage to the bone at the front of the socket. This is called a 'bony-Bankart' lesion. As the humeral head comes to lie on the front of the socket in a dislocation, the back of the head presses firmly on the front of the socket.
This damages both the head (called a Hill-Sachs depression fracture) and the socket. Both of these lesions mean that future dislocations are more likely to happen as the shoulder tends to get to a position where it can ‘lever itself’ out of joint. If there is significant damage to the socket, you may be advised that a Latarjet procedure is most appropriate. This is an operation first described in France in the 1950s but popularised more recently. It involves a small knuckle of bone, normally present at the front of the shoulder (the coracoid process), being moved to the front of the socket. This makes the socket larger so the head needs to travel further before a dislocation happens. Attached to the coracoid process are two muscles. These muscles are left in place after the transfer and then have two functions. Firstly, they act as a sling in front of the joint to hold the head on the socket (quite possibly the main method by which this operation works). Secondly, muscles give bone a blood supply so enable the newly transferred knuckle of bone to heal onto the front of the socket to make the socket larger. The screws are then redundant but can be left in place. The procedure generally works very well and is particularly indicated for overhead / collision athletes or heavy manual workers. Since the bone is attached by screws (rather than stitches in a Bankart repair), the shoulder can normally be moved earlier in the recovery process so the patient needs less time in a sling, usually just 2 weeks.

Antero-posterior X-ray of the shoulder after arthroscopic Latarjet procedure showing the 2 screws on the front of the glenoid. (courtesy of Dr L Lafosse, Annecy, France)

Bernageau view (X-ray) of the shoulder showing the transferred bone graft on the anterior glenoid, held in place by 2 screws. (courtesy of Dr L Lafosse, Annecy, France)
Spire Elland HospitalElland Lane
Elland
HX5 9EB
For an appointment, telephone:
Clinic bookings on 01422 324 069
Self pay enquiries on 01422 229 597
Main Hospital on 01422 229 632
BMI The Huddersfield Hospital
Birkby Hall Road
Huddersfield
West Yorkshire
HD2 2BL
Reception: 01484 533 131
Department of Orthopaedics & Trauma
Calderdale and Huddersfield NHS Foundation Trust
Huddersfield Royal Infirmary
Acre Street
Lindley
Huddersfield
HD3 3EA
NHS Secretary:
Mrs Margaret Thomas
Tel 01484 342 343
NHS Clinics Trauma:
Calderdale Royal Hospital (Halifax) and
Huddersfield Royal Infirmary
Elective Shoulder and Elbow problems:
Friday morning at Calderdale Royal Hospital, Halifax
|